Appendicitis - sounds like one of those emergency-room things no one thinks about until it hits. But it’s more common than you’d guess. It starts when the appendix, a small organ near your large intestine, gets blocked and inflamed. Left untreated, it can rupture - and that’s where things get serious.
This blog unpacks what is appendicitis, the early warning signs, major causes, and what treatment looks like. Whether you’re revising for physiology or just wondering why lower-right belly pain isn’t going away - this guide has you covered in a clear, student-friendly way.
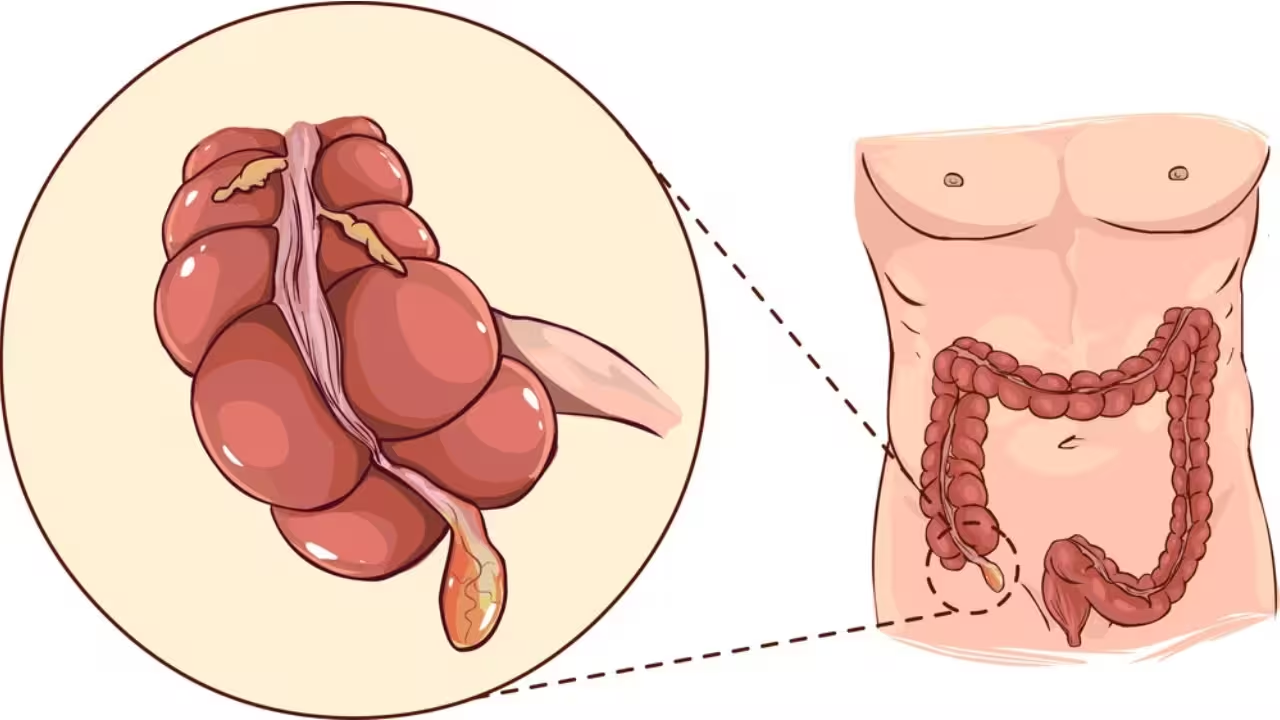
What Is Appendicitis? – Let’s Start With the Basics
Appendicitis is a condition where the appendix - a small, tube-shaped pouch attached to the beginning of the large intestine - becomes swollen and inflamed. It’s often caused by a blockage inside the appendix, which leads to a build-up of bacteria, infection, and eventually pus.

The appendix itself doesn’t serve any major purpose in the body, but when it gets infected, it can cause severe pain and health risks. If left untreated, the inflamed appendix can burst (rupture), spilling infected material into the abdominal cavity - a life-threatening condition known as peritonitis.
There are two types of appendicitis:
- Acute appendicitis: The more common and serious form, where symptoms appear suddenly and worsen quickly.
- Chronic appendicitis: Less common, with mild, long-lasting symptoms that come and go.
The most effective solution is surgical removal of the appendix - a procedure known as an appendectomy. It’s safe, widely performed, and prevents any future risk since the body functions just fine without the appendix.
Causes of Appendicitis – Why Does It Even Happen?
So, what actually causes that tiny worm-shaped organ to go rogue and start hurting like crazy? Appendicitis usually kicks in when something blocks the opening of the appendix. That blockage leads to swelling, bacterial buildup, and eventually, a painful infection.
Some common causes of appendicitis are:
- Fecal blockage (aka fecalith) – Hard stool getting stuck in the appendix is one of the most common reasons.
- Gastrointestinal infections – Stomach bugs or viral infections can trigger inflammation in the appendix area.
- Swollen lymph tissues – Especially after infections like flu, dengue, or measles, nearby lymph tissues may swell and clog the appendix.
- Intestinal worms or parasites – Rare, but they can sometimes block the passage.
- Trauma to the abdomen – Any injury might accidentally mess with the appendix, though this is very rare.
Once the opening is blocked, bacteria multiply super fast inside. That turns the appendix into a swollen, pus-filled pocket - and that’s what causes all the pain, nausea, and urgency to get to the hospital.
Also, a low-fiber diet over time may indirectly increase your risk, since it can cause constipation and slower bowel movements - making blockage more likely. So yeah, fiber isn’t just about digestion; it might just save you from a trip to the ER!
Symptoms of Appendicitis – What Does It Feel Like?
Appendicitis pain can feel sneaky at first. You might think it’s just gas, bloating, or something you ate - but the symptoms get worse, fast. Knowing the early warning signs can actually help you catch it before things get serious.
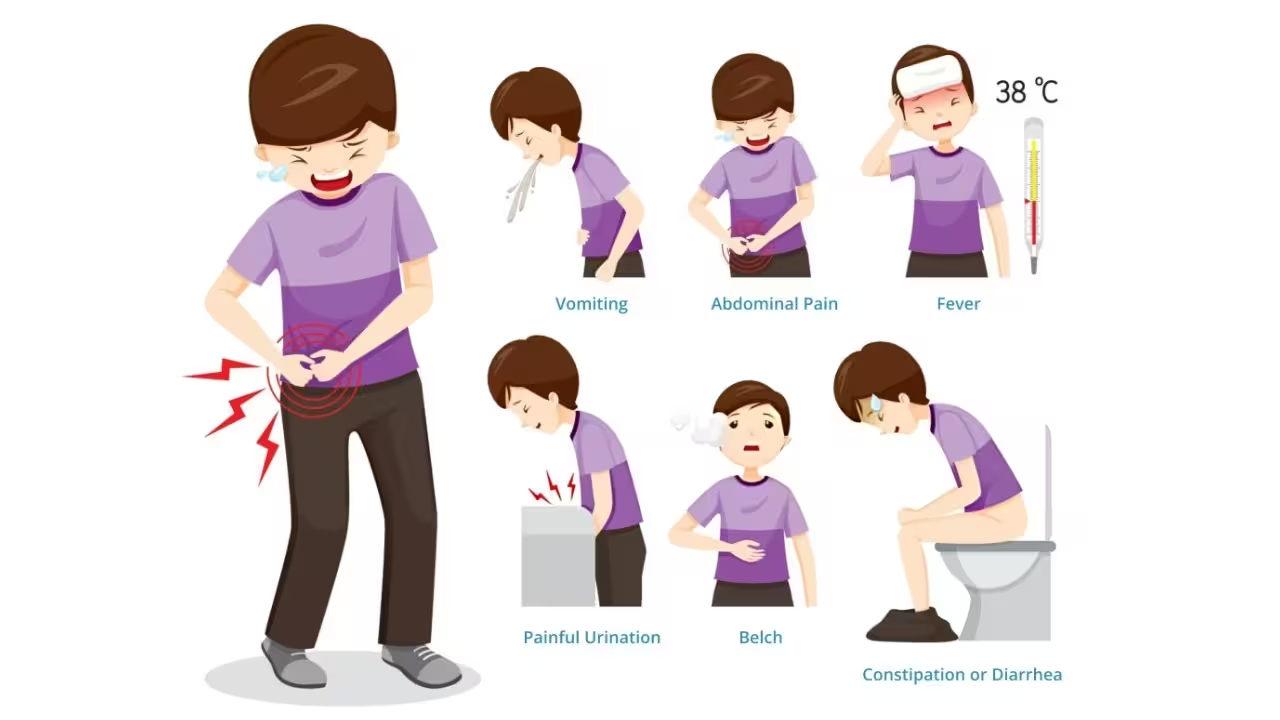
Here are the most common symptoms of appendicitis:
- Pain in the lower right abdomen – It usually starts near the belly button and shifts to the lower right side. This pain keeps getting sharper over time.
- Loss of appetite – Suddenly, you’re just not hungry at all — even your fav snacks won’t tempt you.
- Nausea and vomiting – This usually comes after the pain starts.
- Fever – A mild fever (often around 100–101°F) shows up as the infection builds.
- Bloating or gas – Especially if you can’t pass gas or poop, it might be more than just indigestion.
- Rebound tenderness – If you press your tummy and it hurts more when you let go - that’s a classic sign doctors check for.
Other possible symptoms include diarrhea, constipation, or even pain while urinating (if the appendix is near the bladder).
Important: If the pain keeps increasing and lasts more than a few hours, it’s not something to wait on. Appendicitis can turn into a medical emergency if the appendix bursts - and that’s way more dangerous.
Progression – How Fast Do the Symptoms Get Worse?
Appendicitis doesn’t stay silent for long. Once it starts, things can get serious fast - usually within 24 to 48 hours. That’s why timing is everything.

At first, you might just feel a dull pain near your belly button. It’s mild, confusing, and easy to ignore. But then, the pain shifts to the lower right side of your abdomen and starts getting sharp, steady, and hard to bear.
Here’s how it usually progresses:
- 0–12 hours: Pain begins around the belly button. It feels dull and mild, often mistaken for gas or indigestion.
- 12–24 hours: The pain shifts to the lower right abdomen and becomes sharper. You might feel nausea, a mild fever, or lose your appetite.
- 24–48 hours: Pain intensifies, and vomiting, a higher fever, or swelling in the abdomen can appear. Movement makes it worse.
- After 48 hours: There’s a high risk of rupture, which means the appendix bursts and leaks infection into the abdomen (peritonitis).
If it bursts, it can cause peritonitis (a life-threatening infection) or an abscess - both needing emergency surgery.
So, if someone has stomach pain that keeps getting worse and spreads downward, don’t wait it out. Appendicitis moves quickly, and delays can be dangerous.
Diagnosis – How Do Doctors Confirm It’s Appendicitis?
Doctors don’t rely on just one thing to confirm appendicitis - it’s more like putting together a puzzle. Since the symptoms can sometimes mimic food poisoning, period cramps, or even a UTI, a detailed diagnosis is important before jumping into treatment.

Here’s how the diagnosis usually goes:
- Physical examination
The doctor presses on your lower right abdomen to check for tenderness, pain, or muscle stiffness. Rebound pain (pain when pressure is released) is a key sign.
- Symptom check
You’ll be asked about common signs - like whether the pain started near your belly button and moved to the right, if you're feeling nauseous, vomiting, running a mild fever, or having trouble eating.
- Blood test
A high white blood cell count usually indicates your body is fighting an infection — which supports the suspicion of appendicitis.
- Urine test
This helps rule out other problems like a urinary tract infection or kidney stones, which can have similar symptoms.
- Imaging scans
Doctors usually order an ultrasound or CT scan. These show whether the appendix is swollen or inflamed, and can help confirm the diagnosis before surgery.
- Quick action
If appendicitis is confirmed, treatment often begins immediately to avoid complications. Sometimes, surgery is recommended even if it’s not 100% confirmed, just to be safe.
Treatment Options – What Happens If You Have It?
If you’re diagnosed with appendicitis, the most common treatment is surgery. It’s called an appendectomy, and it involves removing the inflamed appendix before it bursts.

There are two types of surgeries:
- Laparoscopic surgery (also called keyhole surgery) is done using small cuts. It’s less painful, recovery is faster, and there’s minimal scarring.
- Open surgery is done when the appendix has already ruptured or if there’s a lot of infection. It involves a bigger cut and usually needs more recovery time.
Before surgery, doctors usually give IV fluids and antibiotics to control any infection and prepare your body.
In very rare cases, if the symptoms are super mild and caught very early, doctors might try to treat it with antibiotics first. But most people still need surgery eventually to avoid future flare-ups. After the surgery, you’ll get pain relief and more antibiotics to help your body heal.
Most people stay in the hospital for 1 to 2 days if everything goes smoothly. Recovery takes about 1-2 weeks for laparoscopic surgery and a bit more if it was an open one.
Quick treatment is really important if you wait too long and can cause complications, so doctors act fast for a reason.
Complications If Left Untreated – Not Worth the Risk
Ignoring appendicitis might seem harmless at first, especially if the pain goes away. But that’s actually when things can take a serious turn.

What happens if you ignore it?
- Ruptured Appendix: The inflamed appendix can burst, spilling bacteria and pus into your abdomen. This is extremely painful and can become life-threatening.
- Peritonitis: A serious infection of the abdominal lining. It spreads fast and usually requires emergency surgery and hospitalization.
- Abscess Formation: Sometimes, the body tries to “wall off” the infection, leading to pus-filled pockets. These need to be drained and treated with antibiotics.
- Sepsis: This is a worst-case scenario. The infection enters your bloodstream and spreads to the whole body, which can cause organ failure.
Why acting fast matters:
- Appendicitis can go from mild to dangerous in 24–72 hours
- Pain suddenly disappearing doesn’t always mean recovery - it could mean the appendix has ruptured
Bottom line: Delaying treatment can lead to longer hospital stays, more complications, and a tougher recovery. If symptoms match, get it checked ASAP.
After Surgery – What’s Recovery Like?
Once your appendix is out, the recovery part begins - and don’t worry, it’s usually pretty simple if you follow a few basics. Here's how the whole thing plays out:

1. Hospital Stay
- Laparoscopic surgery (small cuts): You’ll likely go home within 24–48 hours.
- Open surgery or burst appendix: You might stay for 3–5 days under observation.
2. Eating After Surgery
- Day 1: Start with clear liquids (like soup, ORS, coconut water).
- Day 2 onwards: Slowly move to soft, bland food (like khichdi or boiled veggies).
- Avoid spicy, oily, or junk food till your stomach fully settles.
3. Back to Normal Life
- School/College:
- After laparoscopic surgery – usually in 5–7 days
- After open surgery – needs about 2–3 weeks
- Physical activities or sports: Wait 4–6 weeks before doing anything intense.
4. Watch Out For These Signs
Call your doctor if you notice:
- Redness, swelling, or pus around stitches
- Fever or chills after a few days
- Pain getting worse instead of better
- Nausea or vomiting returning suddenly
5. Quick Tips for Healing Faster
- Take all medicines on time (especially antibiotics)
- Rest well and don’t lift heavy objects
- Keep the wound clean and dry
- Go for all follow-up checkups without skipping
- Eat light, nutritious food to help your body heal
How to Prevent Appendicitis – Can You Really Avoid It?
Okay, real talk - there’s no 100% way to stop appendicitis, but there are a few simple habits that can lower your risk. It mostly comes down to what you eat and how your gut behaves.

Fiber = Your Friend
- A low-fiber diet = more chance of constipation = blockage in your appendix.
- Try to eat more of:
- Fresh fruits (papaya, guava, apples with peel)
- Leafy greens (palak, methi, lettuce)
- Whole grains (brown rice, oats, atta roti)
Stay Hydrated
- Drink enough water every day. It keeps digestion smooth and prevents buildup in your gut.
- Coconut water, lemon water, and plain water are best - skip sugary soft drinks.
Don’t Ignore Bathroom Signals
- Holding in your poop regularly - more chance of blockage in intestines.
- Go when you need to go. Seriously.
Limit Junk and Processed Food
- Too much oily, fried, and processed stuff can cause long-term stomach irritation.
- It's okay once in a while, but don’t make it your everyday diet.
Bonus Tip: Know Your Body
- If you often get stomach cramps, feel bloated, or have digestion issues - don’t ignore it.
- Keep an eye on any unusual abdominal pain, especially on the right side.
To sum it up: You can’t totally prevent appendicitis, but keeping your stomach happy with a high-fiber diet, lots of water, and regular habits makes a big difference.


.svg)










.avif)








