Blood might seem like a simple topic, but it’s actually one of the most important parts of your body. It’s the fluid that keeps everything running - red blood cells carry oxygen, white blood cells fight infections, and platelets help your body stop bleeding and heal.
In this blog, we’ll break down what blood is, its components, the main functions of blood, common disorders, blood groups, and even how doctors test and monitor it. Whether you’re revising for exams or just curious about how your body works, we’ve explained it all in a simple, student-friendly way.
What is Blood? – Definition & Basic Composition
Blood is the body’s delivery system - a fluid that keeps everything running smoothly. It flows through veins and arteries, carrying oxygen, nutrients, hormones, and even waste products. Without it, none of your organs would get what they need to function properly.

Think of it as a moving highway inside you - where every cell gets what it needs and sends back what it doesn’t. This red liquid isn’t just one thing though; it’s made of several components, each doing a specific job.
Components of Blood
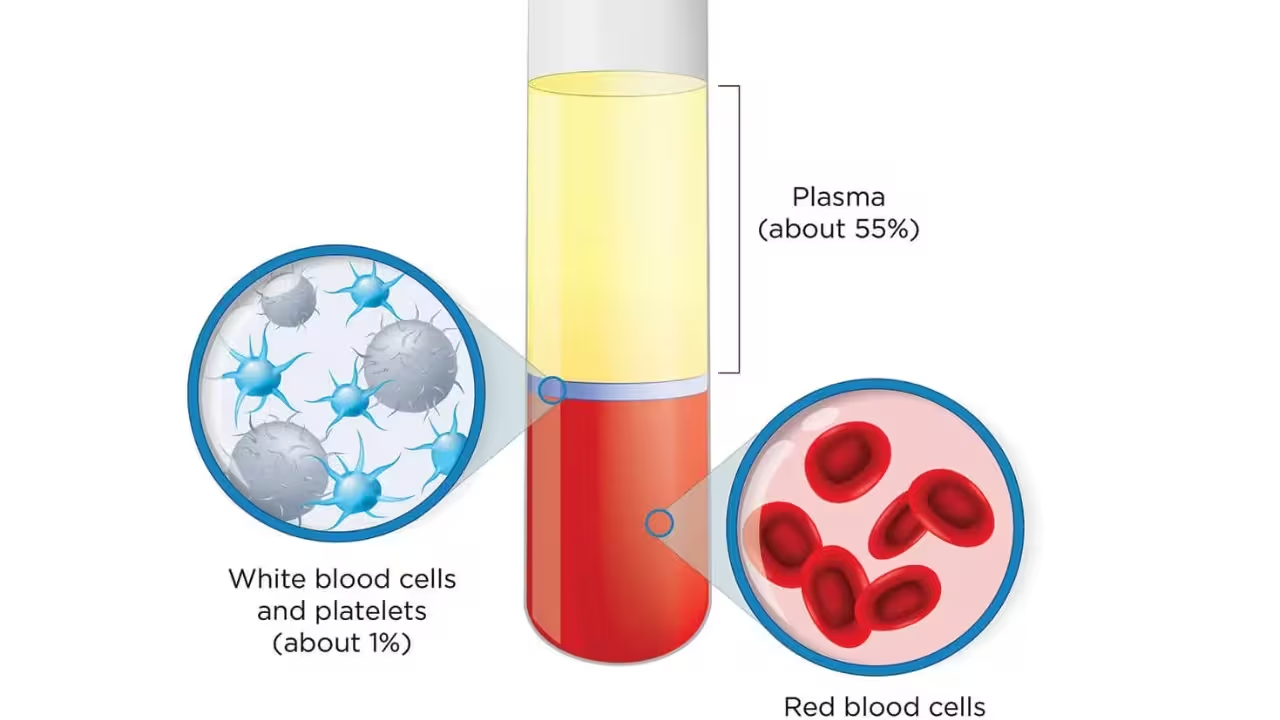
- Plasma (about 55% of total blood): The liquid portion that transports nutrients, hormones, and waste. It contains water, proteins (like albumin and fibrinogen), salts, and antibodies that help maintain pH and regulate body temperature.
- Red Blood Cells (RBCs): Also known as erythrocytes, these cells carry oxygen from the lungs to tissues using hemoglobin. They are biconcave, lack a nucleus, and give blood its red color.
- White Blood Cells (WBCs): Or leucocytes, they defend the body against infections. WBCs are of two types - granulocytes (neutrophils, eosinophils, basophils) and agranulocytes (lymphocytes, monocytes).
- Platelets: Also called thrombocytes, these tiny cell fragments help in blood clotting, preventing excessive bleeding when an injury occurs.
Functions of Blood – More Than Just Oxygen Transport
Blood is much more than a red fluid flowing through your veins. It acts as a transport system, a protector, and a regulator - all in one. Each component of blood has a role to play in keeping your body healthy and balanced. Here are the key functions of the blood:
1. Transportation of Gases
Blood carries oxygen from the lungs to every part of the body and returns carbon dioxide back to the lungs for exhalation. This is mainly done by red blood cells and their hemoglobin content.
2. Transport of Nutrients and Hormones
Nutrients absorbed from food are carried to cells for energy and growth. Hormones released by glands are transported to their target organs to regulate body functions.
3. Regulation of Body Environment
Blood helps maintain body temperature, pH, and water balance. Plasma proteins, salts, and blood flow work together to keep cells hydrated and stable.
4. Protection Against Infections and Blood Loss
White blood cells defend the body against bacteria, viruses, and other pathogens. Platelets help in blood clotting, preventing excessive bleeding when you get injured. Plasma also carries antibodies that fight infections.
5. Excretion of Waste Products
Blood transports metabolic waste like urea and carbon dioxide to the kidneys and lungs for removal, keeping the body clean and functioning efficiently.
What is Plasma and Its Components
Plasma is the straw-colored liquid part of blood, making up about 55% of total blood volume. It’s mostly water, but it’s far from plain - it carries nutrients, hormones, proteins, and waste products throughout the body. Plasma not only moves things around your body, but it also keeps your blood pressure, pH, and fluid balance steady so everything stays in check.
Here are the main components of plasma and their functions:
1. Water (About 90%)
- Acts as a solvent and medium for transporting all other components.
- Helps regulate body temperature by distributing heat throughout the body.
- Maintains blood volume and ensures smooth blood flow through vessels.
2. Plasma Proteins
- Albumin: Maintains osmotic pressure, preventing fluid from leaking into tissues, and helps transport substances like drugs and hormones.
- Globulins: Include antibodies that defend against infections and transport proteins for lipids and metal ions.
- Fibrinogen: Essential for blood clotting, forming a mesh that stops bleeding when vessels are injured.
3. Nutrients
- Glucose, amino acids, fatty acids, vitamins, and minerals travel in plasma to reach cells for energy production, growth, and repair.
- Supplies cells with building blocks needed for enzymes, hormones, and structural proteins.
4. Hormones
- Chemical messengers released by glands, carried by plasma to target organs.
- Regulate growth, metabolism, reproduction, and stress responses.
5. Electrolytes & Salts
- Sodium, potassium, calcium, chloride, and bicarbonate maintain pH, osmotic balance, and proper nerve and muscle function.
- Essential for enzyme activity and overall cellular health.
6. Waste Products
- Urea, creatinine, and carbon dioxide are carried to the kidneys, lungs, and liver for excretion.
- Prevent accumulation of toxins, keeping the internal environment stable.
Types of Blood Cells: RBCs, WBCs, and Platelets
Blood isn’t just a red liquid - it’s a mix of specialized cells, each doing a crucial job to keep you alive and healthy. These cells float in plasma and perform tasks like carrying oxygen, fighting infections, and healing wounds.
Here’s a quick breakdown:
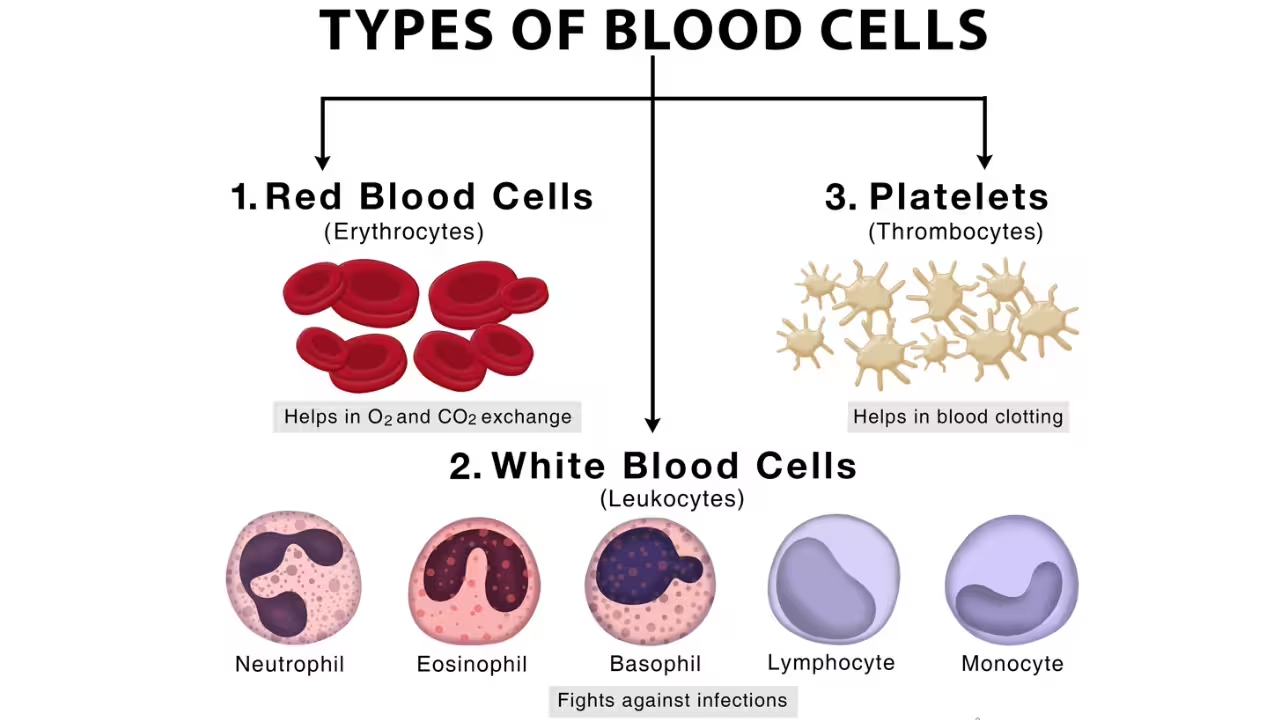
1. Red Blood Cells (RBCs / Erythrocytes)
- Carry oxygen from the lungs to body tissues and carbon dioxide back to the lungs.
- Contain hemoglobin, which binds oxygen and gives blood its red color.
- Biconcaves are in shape and lack a nucleus to maximize space for hemoglobin.
- Normal count: 4.5–5.5 million/mm³; lifespan ~120 days.
2. White Blood Cells (WBCs / Leukocytes)
- Defend the body against infections and foreign substances.
- Normal count: 4,000–11,000/mm³.
- Two main types:
- Granulocytes: Include neutrophils, eosinophils, and basophils; fight bacteria, parasites, and control allergies.
- Agranulocytes: Include lymphocytes and monocytes; regulate immunity and engulf pathogens.
3. Platelets (Thrombocytes)
- Small cell fragments that help in blood clotting and prevent excessive bleeding.
- Formed from megakaryocytes in the bone marrow.
- Normal count: 1.5 - 4 lakh/mm³; low count = thrombocytopenia, high count = risk of unwanted clots.
Together, these cells keep your body running smoothly - transporting oxygen, fighting diseases, and repairing damage whenever needed.
Hemoglobin and Oxygen Transport
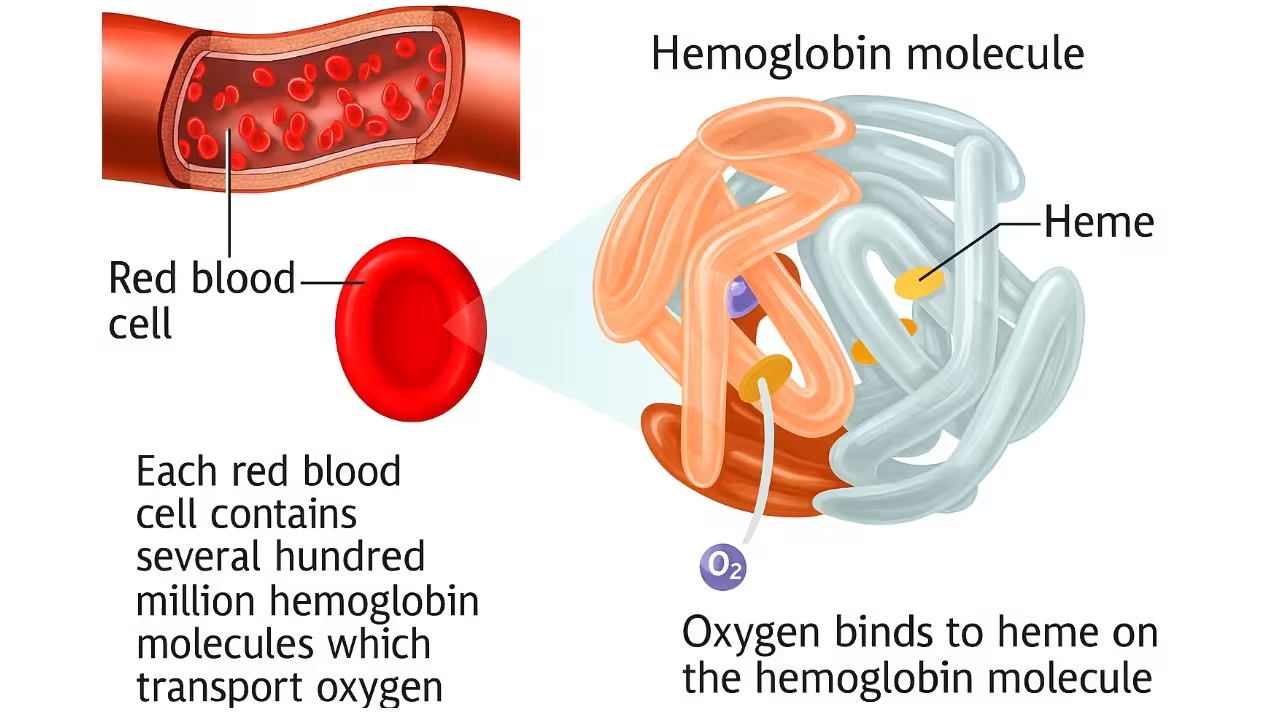
Hemoglobin is a protein found in red blood cells that makes blood red and carries oxygen from the lungs to all body tissues. It also helps transport carbon dioxide back to the lungs for exhalation. Without hemoglobin, your cells wouldn’t get the oxygen they need, and energy production would be affected.
Key Points About Hemoglobin and Oxygen Transport
- Structure of Hemoglobin: Made of four protein subunits, each with an iron-containing heme group that binds oxygen molecules.
- Oxygen Transport: Hemoglobin picks up oxygen in the lungs, binds it, and delivers it to tissues where oxygen is released for cellular respiration.
- Carbon Dioxide Transport: Hemoglobin also carries a portion of carbon dioxide from tissues to the lungs, helping maintain blood pH.
- SpO₂ Levels: The oxygen saturation (SpO₂) indicates how much hemoglobin is carrying oxygen. Normal levels are typically 95–100%.
- Clinical Importance: Low hemoglobin levels can cause anemia, leading to fatigue and shortness of breath. High levels may indicate dehydration or other conditions.
Blood Groups and Blood Typing (ABO and Rh Systems)
Human blood is categorized into different groups based on the presence or absence of specific antigens on the surface of red blood cells. The two primary systems used for blood grouping are the ABO system and the Rh system. Knowing these systems is crucial for safe blood transfusions, organ transplants, and prenatal care.
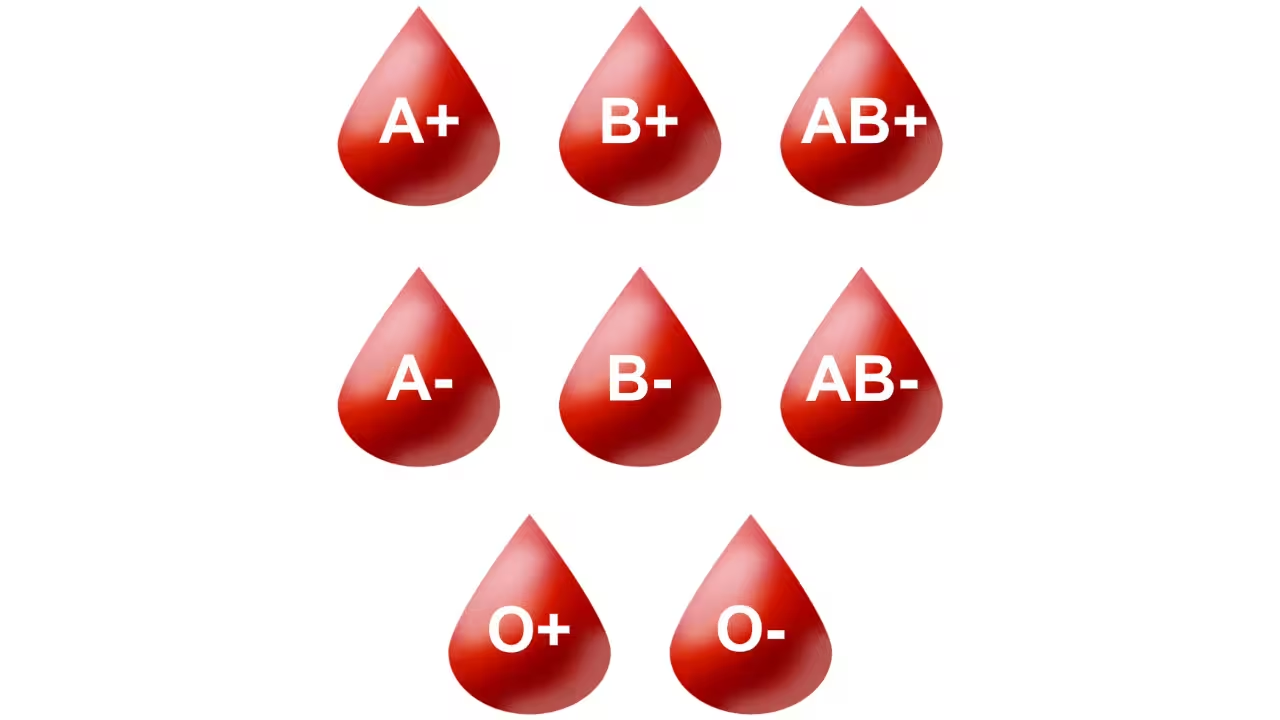
ABO Blood Group System
The ABO system classifies blood based on the presence or absence of A and B antigens on red blood cells and the corresponding antibodies in plasma.
Rh Factor
- The Rh factor is another antigen found on the surface of red blood cells.
- If the Rh antigen is present, the individual is Rh-positive (Rh⁺); if absent, the individual is Rh-negative (Rh⁻).
- Approximately 80% of humans are Rh-positive.
- Rh compatibility is essential during blood transfusions and pregnancy. For instance, if an Rh-negative mother carries an Rh-positive baby, there could be complications, such as hemolytic disease of the newborn.
Clinical Relevance
- Most common blood group: O⁺
- Most rare blood group: AB⁻
- Universal donor: O⁻ (can donate to any blood group)
- Universal recipient: AB⁺ (can receive from any blood group)
Blood Clotting Mechanism: How the Body Stops Bleeding
When a blood vessel is damaged, the body activates a clotting system to prevent excessive blood loss. This involves platelets, plasma proteins, and a series of reactions that form a stable clot while the tissue heals.
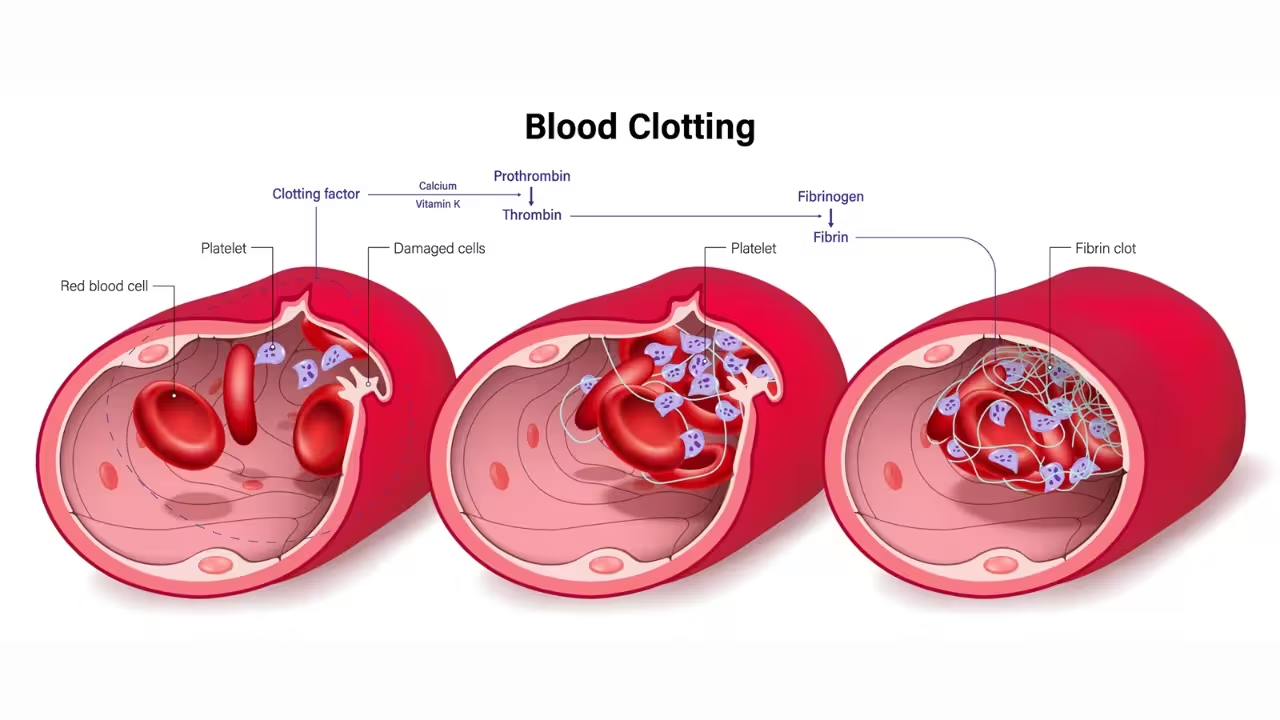
How Blood Clotting Happens
- Vascular Spasm: The damaged vessel constricts to reduce blood flow immediately after injury.
- Platelet Plug Formation: Platelets stick to exposed collagen fibers at the injury site and release chemicals that attract more platelets, forming a temporary plug.
- Coagulation (Clot Formation): Plasma clotting factors activate in a cascade, converting fibrinogen into fibrin threads. These threads weave through the platelet plug to form a strong, stable clot.
- Clot Retraction and Tissue Repair: The clot contracts, pulling wound edges together. Over time, tissue repair occurs, and the clot is gradually dissolved.
Key Points
- Low platelets or deficient clotting factors can cause excessive bleeding (seen in hemophilia).
- Proper clotting protects against blood loss and infection.
- Platelets, fibrin, and clotting factors all work together for effective hemostasis.
Disorders Related to Blood
Blood is vital for carrying oxygen, fighting infections, and clotting when you get injured. But sometimes, blood components don’t work properly, leading to various disorders. Here are some common blood disorders:
- Anemia
Low red blood cell count or hemoglobin reduces oxygen delivery to tissues. It can cause fatigue, weakness, and pale skin. Iron deficiency, vitamin B12 deficiency, or genetic conditions like thalassemia are common causes.
- Leukemia
A type of cancer affecting white blood cells (lymphocytes). It leads to frequent infections, weakness, and bleeding problems because the body produces abnormal WBCs that don’t function properly.
- Hemophilia
A genetic disorder in which blood fails to clot properly due to missing clotting factors. Even small injuries can result in prolonged bleeding.
- Thalassemia
An inherited condition where hemoglobin production is abnormal, causing destruction of RBCs and anemia. Symptoms include fatigue, pale skin, and delayed growth.
- Thrombocytopenia
A low platelet count that can cause easy bruising and excessive bleeding. It may occur due to infections, medications, or bone marrow disorders.
- Polycythemia
A disorder with high red blood cell count, which thickens the blood and increases the risk of clotting or stroke.
Knowing these disorders helps you learn how blood components work together to keep the body healthy. Problems with RBCs affect oxygen transport, WBC issues weaken immunity, and platelet or clotting factor deficiencies impact bleeding control.
Blood Transfusion and Compatibility
A blood transfusion is the process of transferring blood or its components from one person to another. It’s essential when someone loses blood due to injury, surgery, or certain diseases. But not all blood types are compatible - giving the wrong type can trigger serious reactions.
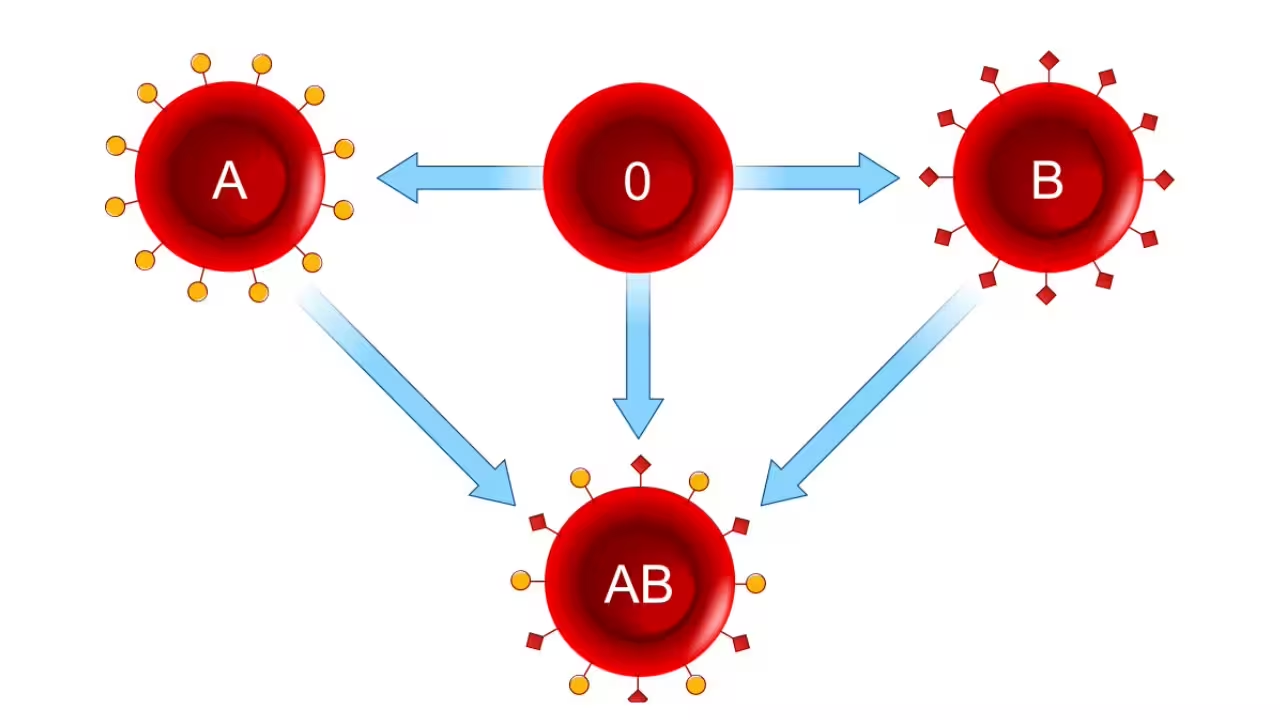
Important Points About Blood Transfusion
1. ABO Compatibility:
- Type O is the universal donor (can donate to A, B, AB, O).
- Type AB is the universal recipient (can receive from all types).
2. Rh Factor Compatibility:
- Rh-negative individuals should not receive Rh-positive blood.
- Rh-positive people can receive both Rh-positive and Rh-negative blood.
3. Platelets and Plasma:
- Platelet transfusions help in bleeding disorders or low platelet count.
- Plasma transfusions provide clotting factors and help in conditions like hemophilia.
4. Special Blood Types:
- Bombay blood group is very rare; compatibility is extremely limited.
- Always check both ABO and Rh type before transfusion.
Correct transfusions save lives by restoring oxygen delivery, immunity, or clotting ability, while wrong transfusions can cause reactions ranging from fever to life-threatening hemolysis.
Blood Volume Regulation
Keeping blood volume within the right range is crucial for healthy circulation and maintaining blood pressure. The body uses several systems that work together to balance blood volume.
1. Kidneys and Renin-Angiotensin System
The kidneys sense changes in blood pressure and volume. They release renin, which triggers angiotensin activation, causing the body to retain water and salt, increasing blood volume.
2. Antidiuretic Hormone (ADH)
Produced by the pituitary gland, ADH tells the kidneys to retain water, helping prevent dehydration and maintain proper blood volume.
3. Atrial Natriuretic Peptide (ANP)
Secreted by the heart’s atria when blood volume is high. ANP promotes excretion of sodium and water through urine to reduce blood volume.
4. Thirst Mechanism
When blood osmolarity rises, it triggers thirst, prompting you to drink water and restore blood volume.
5. Fluid Shifts Between Blood and Tissues
Water moves between blood vessels and surrounding tissues based on osmotic and hydrostatic pressures, helping maintain a balanced blood volume.
Blood pH and Buffer Systems
Blood must stay slightly alkaline, around pH 7.35 - 7.45, for the body to function properly. Imagine it like a balancing act: every time acids or bases enter the blood, the body quickly steps in to keep things stable.
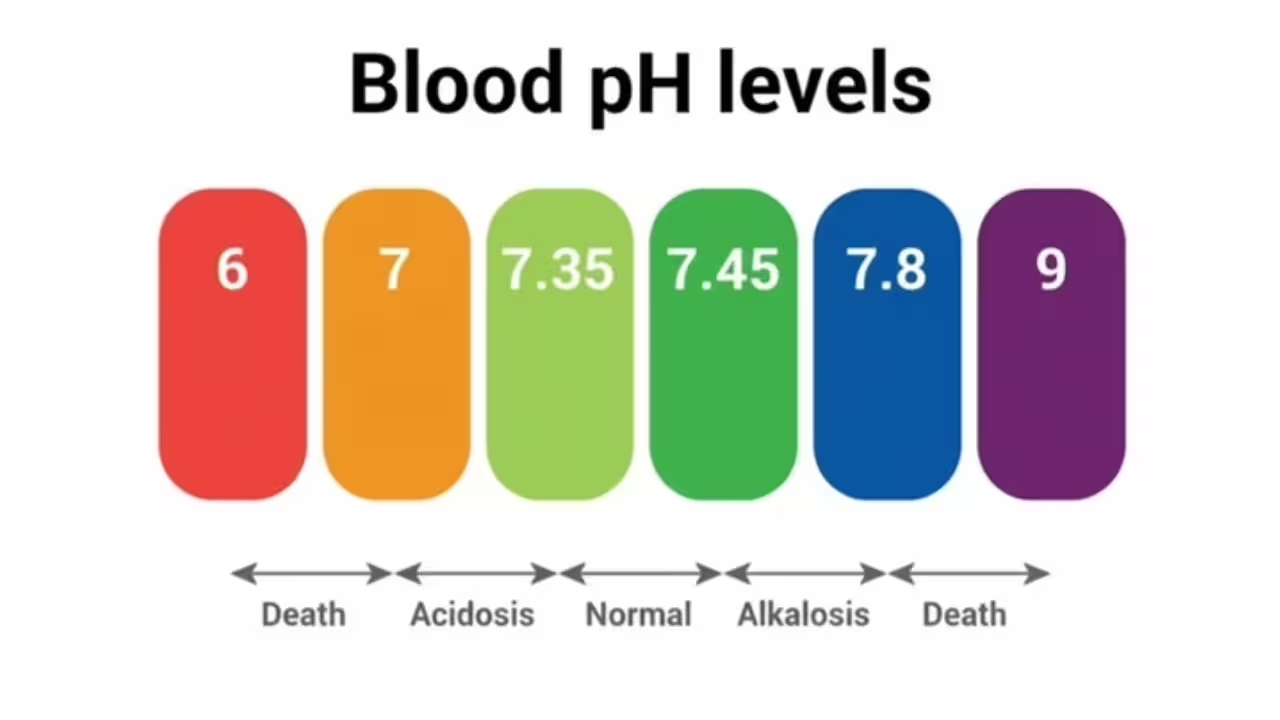
- When acid levels rise, the bicarbonate buffer grabs extra H⁺ ions and forms carbonic acid, preventing pH from dropping.
- If blood becomes too basic, the same buffer releases H⁺ ions to bring pH back to normal.
- Proteins like hemoglobin also act as mini-buffers, binding or releasing H⁺ inside red blood cells.
- Phosphate buffers work mainly inside cells and in urine, adding another layer of protection.
- On top of that, the lungs adjust CO₂ levels by breathing faster or slower, helping control acidity quickly.
- Kidneys handle long-term adjustments, excreting hydrogen ions and reclaiming bicarbonate to keep blood pH steady over days.
Think of it like a team effort: buffers handle immediate changes, lungs react fast to CO₂, and kidneys make long-term corrections. Together, they ensure your blood stays in the perfect pH range for all the cells and enzymes to work.
Role of Blood in Immunity
Blood isn’t just about carrying oxygen or nutrients - it’s also one of the body’s main defense systems. Every drop of blood carries cells and proteins that constantly guard you against infections, viruses, and other harmful substances. Together, they form your immune response, which detects, attacks, and remembers any invading germ that tries to enter the body.
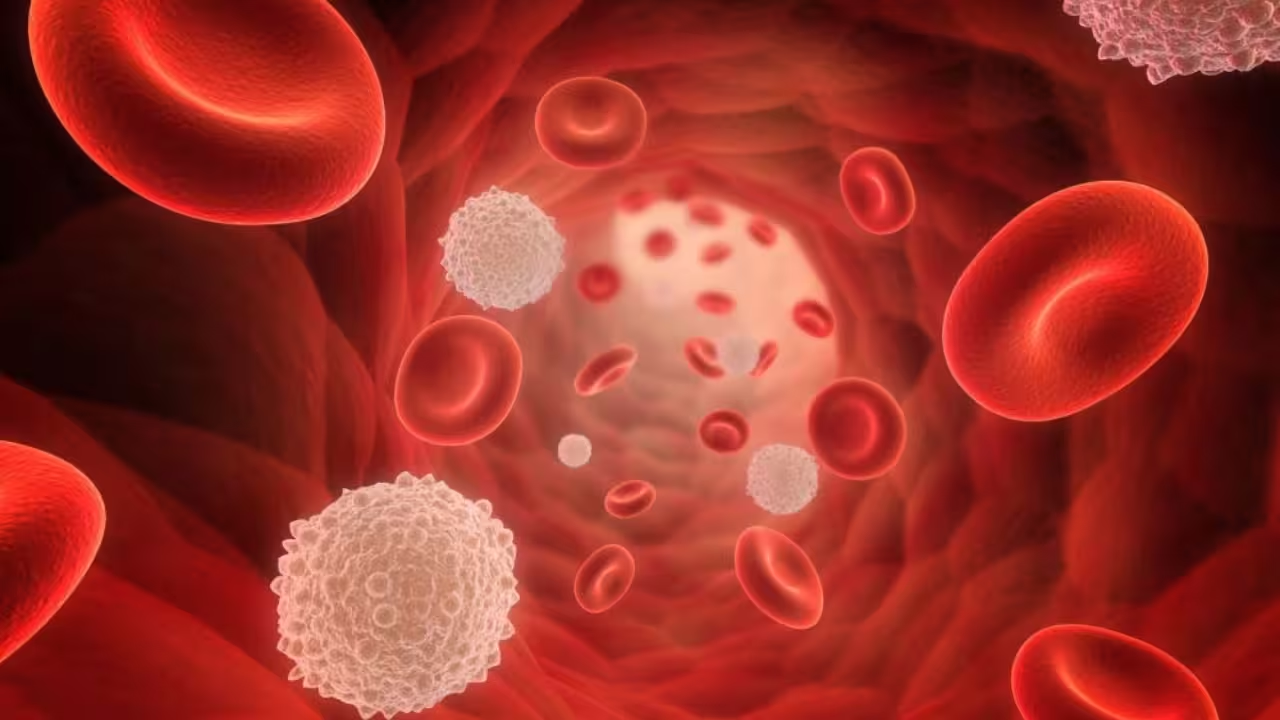
1. Detecting Germs
Some white blood cells, like lymphocytes and monocytes, are always on the lookout for bacteria, viruses, or any foreign particles that enter the body.
2. Quick Defence
When an infection begins, neutrophils reach the affected area first. They surround and destroy germs through a process called phagocytosis - basically “eating up” the invaders.
3. Coordinated Attack
Then come the lymphocytes.
- B-lymphocytes produce antibodies that lock onto pathogens and neutralize them.
- T-lymphocytes destroy infected cells directly to stop the spread of infection.
4. Building Immunity
After recovery, some lymphocytes stay back as memory cells. They help the body respond faster if the same infection happens again - that’s how long-term immunity develops.
5. Support from Plasma and Platelets
The plasma part of blood carries antibodies, complement proteins, and cytokines, which make the immune response stronger. Even platelets help by releasing chemicals that signal immune cells when there’s an injury or infection.
So, while we usually think of blood as a transporter, it’s actually a big part of our immune defense system, quietly protecting us every day
Blood Circulation in Humans
The human body has a closed circulatory system, which means blood flows continuously within blood vessels, pumped by the heart. This system ensures every cell gets oxygen and nutrients while removing waste products like carbon dioxide.
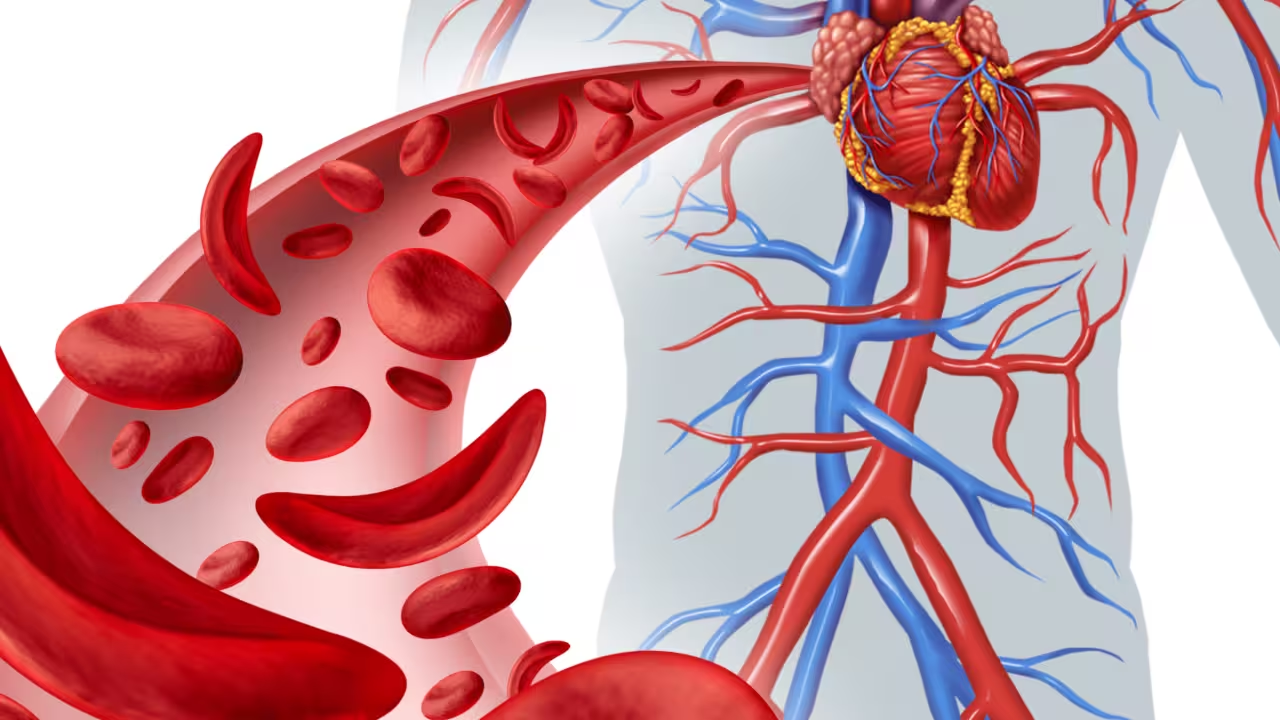
1. The Starting Point – The Heart
The heart is the central pump of the circulatory system. It has four chambers - two atria (upper chambers) and two ventricles (lower chambers). The right side handles deoxygenated blood, while the left side pumps oxygenated blood.
2. The Path of Blood Flow
- Deoxygenated blood from the body enters the right atrium → moves to the right ventricle → and is sent to the lungs through the pulmonary arteries.
- In the lungs, blood releases carbon dioxide and absorbs oxygen.
- Oxygenated blood then returns to the left atrium → moves to the left ventricle → and is pumped out to the entire body through the aorta.
3. Types of Circulation
- Pulmonary Circulation: Movement of blood between the heart and lungs.
- Systemic Circulation: Circulation between the heart and the rest of the body. Together, these two types ensure oxygen reaches every tissue and waste is efficiently removed.
4. The Role of Blood Vessels
- Arteries carry blood away from the heart (usually oxygen-rich).
- Veins carry blood toward the heart (usually oxygen-poor).
- Capillaries are tiny vessels where oxygen, carbon dioxide, and nutrients are exchanged between blood and tissues.
Proper circulation keeps the body’s cells alive and functioning. If blood flow stops even for a few minutes, tissues begin to die due to lack of oxygen - showing how vital this system truly is.
Diagnostic Tests Involving Blood (CBC, ESR, etc.)
Imagine you go to a doctor for a routine checkup or because you feel unwell. The doctor orders some blood tests - here’s what each one tells you:

- Complete Blood Count (CBC)
If you’re feeling tired or weak, a CBC can reveal whether your red blood cells are low (anemia) or if your white blood cells are high (infection). Platelet count is checked too, to see if your blood can clot normally.
- Erythrocyte Sedimentation Rate (ESR)
Say you have body pain or inflammation. The ESR test shows how fast your red blood cells settle. A faster rate usually signals inflammation somewhere in your body, helping doctors pinpoint issues.
- Hemoglobin Test
If you’re short of breath or dizzy, a hemoglobin test will check how much oxygen your blood can carry. Low hemoglobin means anemia, while high levels may indicate dehydration or other conditions.
- Blood Glucose Test
If you feel unusually thirsty or tired, a blood glucose test can detect high sugar levels, which could point to diabetes.
- Blood Typing
Before any transfusion, doctors need to know your ABO and Rh blood group to ensure compatibility. The wrong type can cause serious reactions.
- Platelet Count and WBC Count
If you bruise easily or get frequent infections, these tests help. Low platelets can mean bleeding problems, while abnormal white blood cell counts may suggest infection or immune issues.


.svg)










.avif)








