Allergy and autoimmunity - words you’ve probably heard when someone keeps sneezing or has long-term health issues. But it’s way more than just being sensitive or sick. These happen when your immune system overreacts or turns against your own body. and that affects everything from your skin to your energy.
This blog breaks down what is an allergy, what is autoimmunity, their causes, symptoms, types, and what happens if they’re left untreated. Whether you’re prepping for exams or just trying to figure out why your immune system is misfiring - this is your one-stop, student-friendly guide.
Understanding the Immune System and Why It Acts Like a Bodyguard
Your immune system works like a full-time bodyguard - always on duty to protect you from harmful stuff like viruses, bacteria, and toxins. It’s built to recognize what’s “you” and what’s not, so it can attack invaders without hurting your own body. That ability to tell self from non-self is super important - when it fails, problems like autoimmunity or allergies happen.
The immune system has two main parts:
- Innate immunity: this is your fast, first line of defense. It reacts quickly to anything suspicious (like skin, mucus, and general white blood cells).
- Adaptive immunity: this one learns. It creates specific antibodies and remembers past infections so your body can fight them faster next time.
When both parts work well together, you stay healthy. But when this system overreacts or misfires, it can start treating harmless things (like pollen or food) as threats - or even attack your own cells.
What Is an Allergy? And Why Your Body Freaks Out Over Dust
Allergy sounds like just a fancy way to say “I sneeze around cats,” but it’s actually your immune system going full heavy mode over something totally harmless. Basically, your body sees things like pollen, dust, certain foods, pet hair, or insect stings as dangerous invaders - even though they’re not.

Here’s what happens:
Your immune system mistakes these normal things (called allergens) as threats, and reacts with a full-blown defense - often way more intense than needed. That’s why you end up with:
- Sneezing and runny nose
- Itchy skin or eyes
- Rashes or swelling
- Breathing issues in severe cases
Some people deal with mild seasonal sniffles, while others go into anaphylactic shock, which is life-threatening and needs instant medical help.
So next time someone says, “It’s just a peanut,” remember - for someone with a peanut allergy, it’s a full-on immune battle inside.
How Allergic Reactions Actually Work – IgE, Histamine & Chaos
Allergic reactions are basically your immune system overreacting to things that are usually harmless - like pollen, pet hair, or certain foods. so, what really happens inside your body during an allergy attack? It’s all about your immune system reacting when it doesn’t need to.
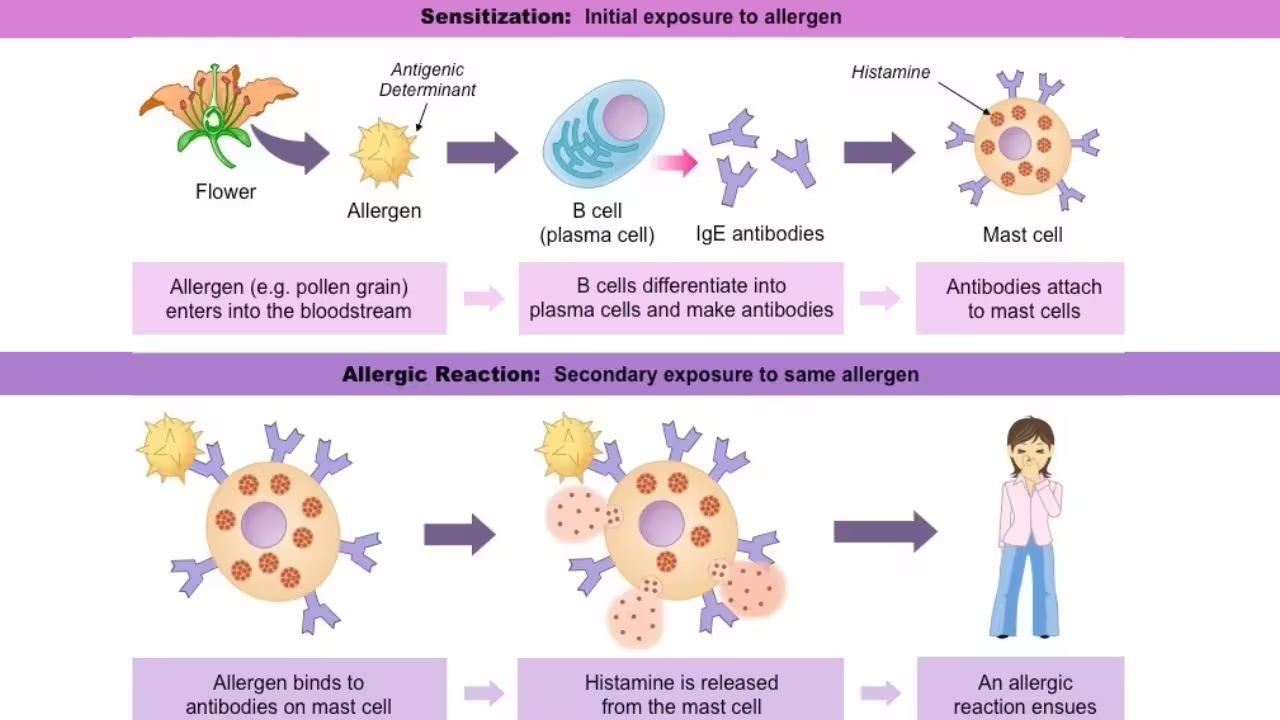
Here’s a simple breakdown:
- When you're first exposed to something like dust, pollen, or peanuts (called an allergen), your body mistakenly sees it as a threat.
- In response, your immune system produces IgE antibodies - these are proteins meant to fight off harmful invaders.
- These IgE antibodies attach themselves to mast cells, which are found in areas like your nose, skin, and lungs.
- The next time that allergen enters your body, those mast cells release histamine and other chemicals.
- This causes allergy symptoms like sneezing, rashes, watery eyes, or even breathing trouble.
You can think of histamine as the reason behind most allergy symptoms - it causes swelling, irritation, and inflammation.
There are two main types of allergic responses:
- Immediate: Starts within minutes (like food allergies or insect stings)
- Delayed: May take hours to show (like some skin rashes)
And yes, the severity can go from mild itching to serious conditions like anaphylaxis, which needs emergency care.
Symptoms of Allergies – From Itchy Eyes to Full-Blown Shock
Allergies can show up in a bunch of different ways depending on the trigger and how sensitive your body is. Some people just sneeze a little, others might end up in the ER. That’s how wide the range is.
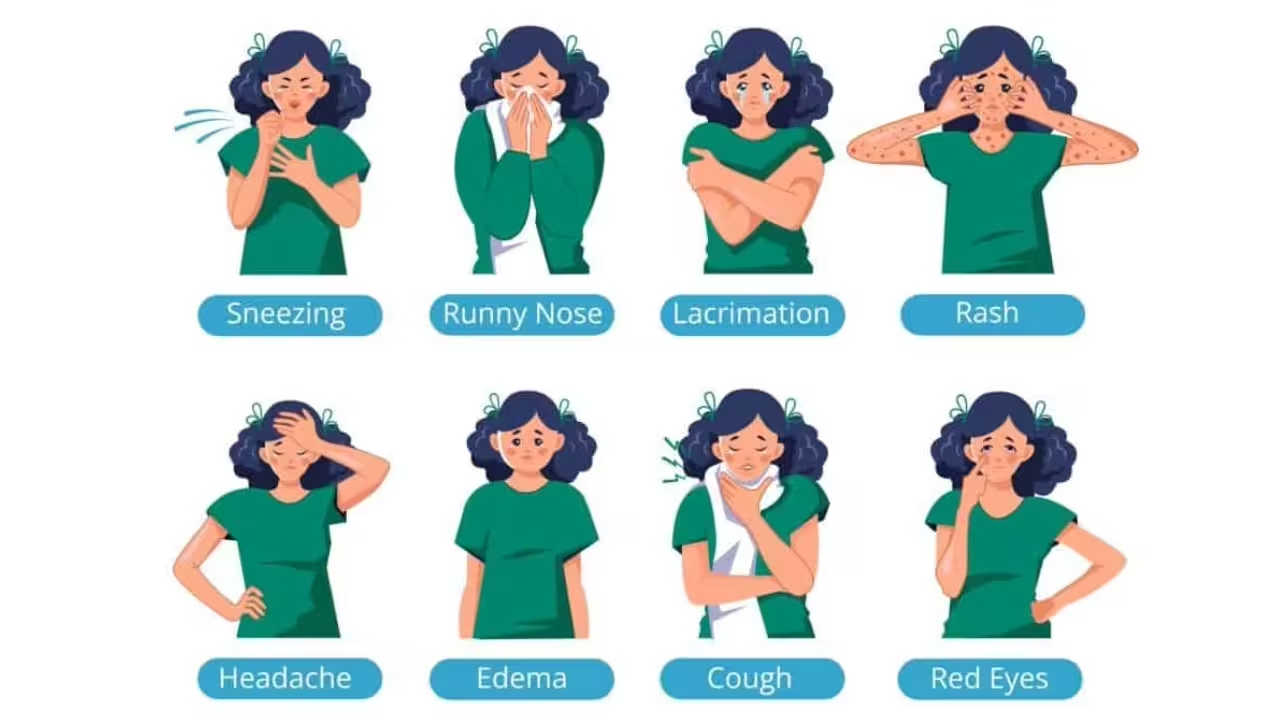
Mild to Moderate Symptoms (Common in Daily Allergies)
These usually pop up with things like dust, pollen, or certain foods:
- Sneezing, stuffy or runny nose (classic hay fever)
- Itchy or watery eyes (especially during allergy season)
- Skin rashes or hives (like red, itchy patches)
- Coughing or mild wheezing (your airways reacting)
- Itchy throat or ears
- Digestive issues like cramps or bloating (mainly food allergies)
These symptoms are uncomfortable but not usually dangerous. Over-the-counter meds like antihistamines or nasal sprays usually help manage them.
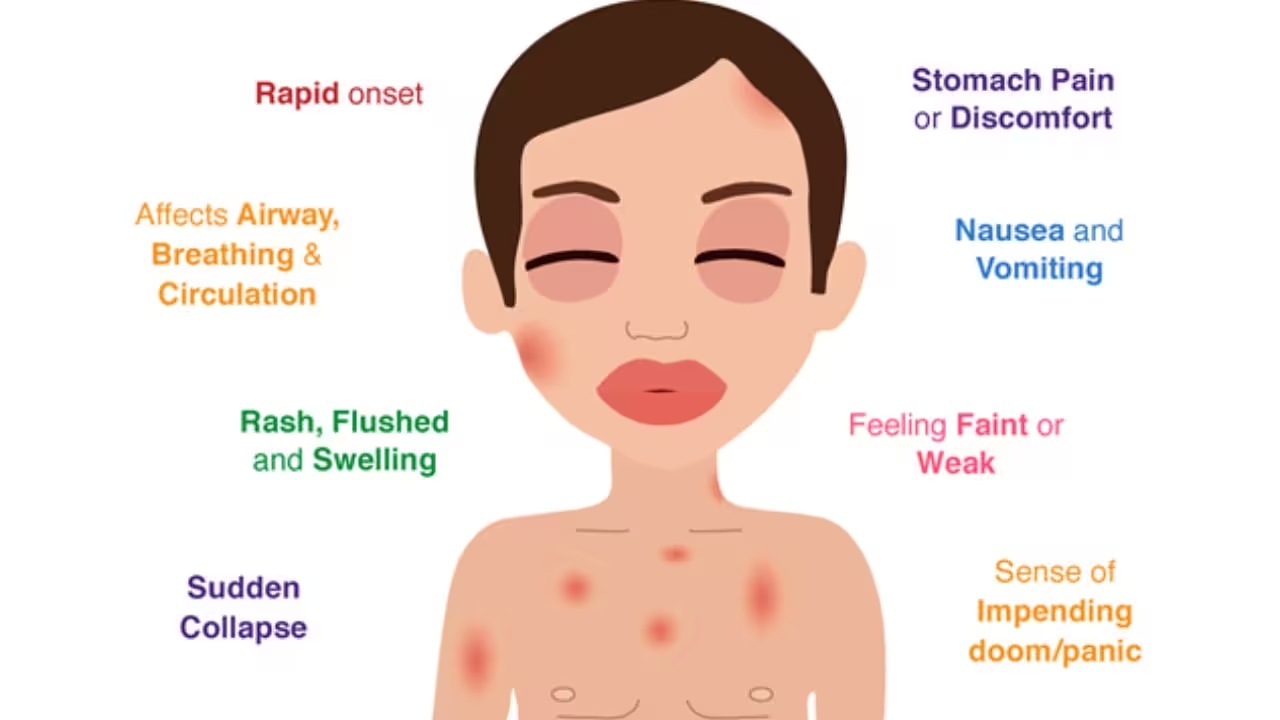
Severe Symptoms – Anaphylaxis (Emergency Case)
This is where things get serious. Anaphylaxis is a life-threatening allergic reaction that happens fast and needs emergency care, you can watch for:
- Swelling in lips, face, tongue, or throat
- Breathing trouble or tightness in the chest
- Fast heartbeat, dizziness, or feeling like you’ll faint
- Low blood pressure or sudden confusion
- Nausea, vomiting, or diarrhea
If someone is having these symptoms, they need an epinephrine shot (like an EpiPen) immediately and should go straight to the hospital.
Seasonal vs. Perennial Allergies
- Seasonal allergies happen during specific times (spring pollen, monsoon mold, etc.)
- Perennial allergies last all year (from indoor allergens like dust, pet hair, or cockroaches)
How Doctors Diagnose and Treat Allergies (Not Just Antihistamines)
If you’re constantly sneezing, breaking out in rashes, or avoiding certain foods like the plague, it might be time to figure out what’s actually triggering your immune system. Doctors don’t just guess - they run specific tests to get to the bottom of your allergy drama.

How Allergies Are Diagnosed
Here’s what usually happens at the clinic:
- Skin Prick Test: A tiny drop of suspected allergen is pricked into your skin. If you get a bump or redness, boom - allergy confirmed.
- Blood Test (IgE Test): Checks your blood for allergy-related antibodies (especially Immunoglobulin E).
- Elimination Diet (for food allergies): Doctors may ask you to avoid certain foods and reintroduce them one at a time to track symptoms.
These tests help figure out exactly what you're allergic to, so you can avoid it or treat it better.
Common Allergy Treatments
Managing allergies isn’t just about popping pills. It depends on your symptoms and what’s causing them:
- Antihistamines: Block the chemical (histamine) that causes sneezing, itching, or runny nose.
- Decongestants: Reduce swelling in your nose, helping you breathe easier.
- Corticosteroid sprays or creams: Calm down inflammation in your nose or on your skin.
- Immunotherapy (Allergy shots): If your allergies are really bad and year-round, you might get allergy shots that slowly train your body to stop overreacting.
- Epinephrine (EpiPen): For life-threatening allergic reactions (anaphylaxis), this is your go-to emergency shot.
The goal isn’t just to stop the sneezing - it’s to make your body less reactive over time and prevent dangerous flare-ups.
What Is Autoimmunity? When the Immune System Turns Against You
Autoimmunity isn’t just some complicated biology term - it’s your immune system flipping sides and attacking your own body. Yup, the system meant to protect you ends up mistaking your healthy cells as enemies.
Here’s what goes wrong:
- Normally, your immune system targets only invaders like viruses and bacteria.
- But in autoimmune conditions, it can’t tell the difference between “self” and “non-self.”
- So it starts damaging your own tissues, thinking it’s helping.
Depending on which part of the body it targets, this leads to different diseases like:
- Type 1 diabetes (immune cells attack insulin-making cells),
- Rheumatoid arthritis (targets joints),
- or Lupus, which can mess with multiple organs at once.
It’s chronic, tricky to diagnose, and while there’s no full cure, there are remedies for autoimmune disease like immunosuppressants, lifestyle tweaks, and anti-inflammatory diets that help keep it in check.
So yeah - if you’re wondering what is autoimmunity, just think: your immune system, but confused and accidentally fighting its own team.
Common Autoimmune Diseases You Should Know
Autoimmune diseases come in different forms - some mess with just one organ, others hit multiple systems at once. But what they all have in common is this: your immune system turns into an overzealous warrior and starts harming your own cells.

Here are some major ones you should know:
- Type 1 Diabetes: Immune cells destroy insulin-producing cells in the pancreas. This means blood sugar gets out of control unless managed.
- Rheumatoid Arthritis (RA): The immune system targets joints, causing swelling, pain, and stiffness - especially in the morning.
- Systemic Lupus Erythematosus (SLE): A more complex one. It can attack skin, joints, kidneys, and even the brain.
- Hashimoto’s Thyroiditis: Your thyroid gets attacked, slowing metabolism and causing fatigue, weight gain, and mood swings.
- Multiple Sclerosis (MS): The immune system damages the protective covering of nerves, leading to coordination and vision problems.
Some are organ-specific, while others are systemic (affecting the whole body). That’s why no two autoimmune cases are exactly alike.
Autoimmune conditions may not be curable yet, but cures for autoimmune diseases are being researched every day. For now, early diagnosis and good management make a huge difference.
Why Autoimmunity Happens – Not Just Genetics
Autoimmune diseases aren’t caused by one single thing - they happen when your immune system gets confused and starts attacking your own body. And no, it’s not always genetic.

1. Family History
If someone in your family has an autoimmune disorder (like type 1 diabetes, lupus, or rheumatoid arthritis), your chances go up. But having the gene doesn’t mean you’ll definitely get it.
2. Infections
Some viral or bacterial infections confuse your immune system. Even after you recover, leftover immune cells may start attacking healthy parts of your body.
3. Environmental Triggers
Pollution, certain drugs, or exposure to harmful chemicals may trigger autoimmune responses - especially in people who are already genetically sensitive.
4. Hormones
Women are more likely to develop autoimmune diseases. Hormones like estrogen, and changes during puberty or pregnancy, might play a role.
5. Stress & Gut Health
Poor gut health and long-term stress can weaken immune tolerance, making the body more prone to attacking itself.
So in the end, it’s not just about genes. It’s a mix of body, mind, and environment working (or misfiring) together.
Autoimmune Symptoms – The Ones That Keep Coming Bac
Autoimmune diseases are tricky because their symptoms often come and go - and don’t always look the same in everyone. But when your immune system attacks healthy body parts, it leaves behind some common warning signs.
.avif)
- Constant fatigue – Like, no matter how much you rest, you still feel drained
- Joint pain or stiffness – Especially in the morning or after rest
- Stomach issues – Bloating, cramps, or diarrhea, often seen in gut-related conditions like Crohn’s
- Unexplained rashes or skin changes – Redness, flakiness, or patchy spots
- Hair loss or thinning – Sudden shedding, not linked to stress or diet
- Mild fevers – Coming and going without any infection
- Mood changes or brain fog – Trouble focusing, memory lapses, or low mood
The tough part is these symptoms overlap with many other things, which is why autoimmune conditions often go undiagnosed for a while. But if they keep happening or show up in patterns, it’s time to pay attention and get checked.
Managing Autoimmune Diseases – There’s No Cure, But There’s Hope
Autoimmune diseases don’t have a full-on cure yet, but that doesn’t mean life stops. With the right care, people can live almost normal lives. Here’s how it’s managed:

- Medicines that calm your immune system
Doctors usually give immunosuppressants or steroids to reduce inflammation and stop the immune system from attacking your own body.
- Diet & lifestyle really matter
Many people feel better by avoiding certain trigger foods (like gluten or dairy), sleeping well, and keeping stress levels low.
- Track flare-ups
Keeping a symptom journal helps. You’ll notice patterns - like stress, certain foods, or even weather triggering your symptoms.
- Regular check-ups
Autoimmune conditions can change over time, so doctors may need to adjust your treatment depending on how your body’s reacting.
- No cure, but hope’s real
Flare-ups may come and go, but most people learn how to manage them. It's all about balance and early action.
So no, there’s no cure (yet), but with the right care and consistency, it’s definitely manageable.


.svg)










.avif)









